Postmastectomy lymphedema is a well-known sequelae of breast cancer treatment.
What Occurs During Surgery?
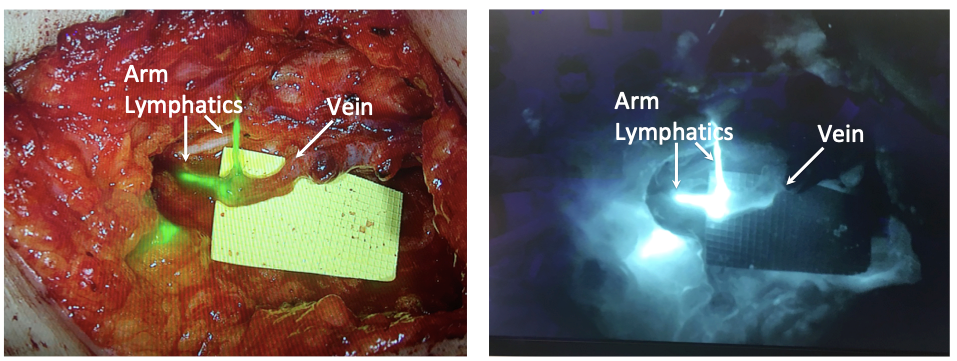
These lymph vessels may be cut during surgery to treat breast cancer, especially if you require an axillary lymph node dissection (removal of lymph nodes in your armpit). As a result, this fluid may not drain as effectively from your arm, leading to lymphedema and swelling. Aside from axillary dissections, patients with a high body-mass index (over 30) or those patients who are undergoing radiation therapy may also be more likely to develop lymphedema after surgery. The swelling that results from lymphedema can be significant, and often interferes with daily activities such as getting dressed or just moving around. Lymphedema also causes your immune system to be less effective at fighting infections in the affected area, meaning that simple cuts, scrapes, or insect bites could turn into something serious. Over time, fibrous and fatty tissue can begin to grow in the affected limbs and make it harder to reverse the swelling.